Emerging Treatments for Coronavirus
ACE Blockers and Coronavirus Infections
David Bishai, MD, MPH, PhD
Johns Hopkins Bloomberg School of Public Health
March 19, 2020
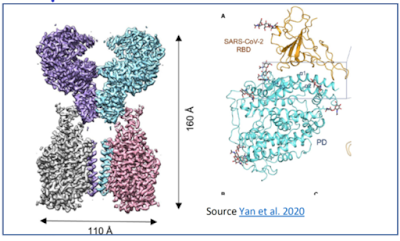
After the SARS-CoV-2
virus gets into a person’s nose, throat,
or lungs it can’t make them sick unless it actually gains entry into the inside
of the epithelial cells that line those tissues. There is a receptor on human
respiratory epithelial cells called the Angiotensin Converting Enzyme 2 (ACE-2).
Its usual job is to cleave proangiotensin into smaller molecules like
angiotensin1-7 that help repair blood vessels in the lung. (McKinney, et al. 2014) The SARS viruses became pathogens when they
mutated to have an affinity for one small spot on human ACE-2 (Figure 1). When ACE-2 receptors are attacked there may
be less angiotensin 1-7 and less ability to repair blood vessels in the lung. Gurwitz (2020)
Figure 1. Electron microgram of the ACE-2 Receptor (Purple and Blue) and SARS-CoV-2 virus (Yellow)
Source Yan
et al. 2020
There is a
much more well known cousin of ACE-2 called ACE-1 which plays an important role
in blood pressure regulation. We have several FDA approved drugs that block
ACE-1 that end in the suffix “sartan” (eg. Losartan and Valsartan). Unfortunately the ACE-1 blocking drugs do not
block ACE-2. Furthermore, when patients take an ACE-1 drug it makes them
express more of the virus-magnet ACE-2 molecule on cell surfaces.
A knee jerk reaction might be to warn doctors: “Do not give Losartan to people during a coronavirus epidemic”. But it is not that simple. Reports from Chinese doctors treating critically ill patients indicate that a mechanism of lung injury during COVID-19 is having too little angiontensin 1-7 and too much pro-angiotensin and byproducts of pro-angiotensin because virus has bound up the ACE-2 receptors. Paradoxically having more ACE-2 receptors during a severe infection might help. Each respiratory cell is going to have some ACE-2 receptors anyway and each cell will be under attack. Having more ACE-2 receptors might not change the outcome of whether virus will invade a respiratory cell, but it might help the body prevent lung injury. (Lowe, 2020) None of this physiology is known with certainty. Trials are underway. We need international cooperation with more centralized health systems like Italy and China to pull of urgent data-mining of COVID-19 patient records.
We don't have answers to pressing questions. Should healthy people who are taking Losartan
anyway stop taking it and switch to something else? Should people who test positive
for COVID-19 and only have mild illness start taking it? What should an ICU doctor do with a critically
ill COVID-19 patient? Which of these
scientific questions should be studied first?

Comments
Post a Comment